Estimated reading time: 0 minutes
Have you lately received an HS diagnosis? You must be both relieved and bewildered. Your ailment has a name…But what exactly is it? We offer the solutions you require.
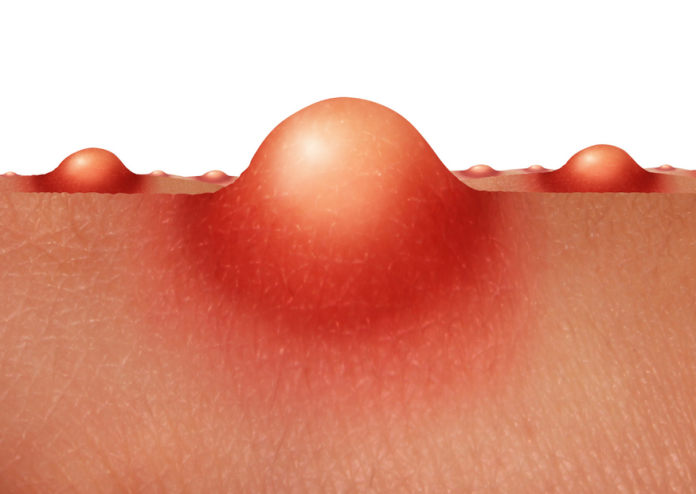
Anyone diagnosed with hidradenitis suppurativa (HS) is sure to have many questions, especially if you’ve never heard of the disease. So let us begin with the most fundamental definition: HS is a chronic inflammatory illness that causes painful lumps, open sores, and permanent scars in the armpits, groyne, buttocks, and beneath the breasts (essentially everywhere the skin rubs together). Now for the additional answers you’re looking for:
Is it my fault I have HS?
No, you are not at fault. For the record, HS does not develop as a result of “bad hygiene,” as some doctors incorrectly (and even violently) claim. Such guilt-tripping, according to Dr. Adil, is “deeply unfair” because “none of us fully understands where HS comes from.”
So, what do we know about HS’s causes?
“We’re still trying to understand the fundamental mechanisms behind HS,” says Dr. Adil Ayurveda Skin Specialist, who runs an HS clinic in Bangalore, India. We do know that people with HS have inflammation around their hair follicles, especially in the intertriginous zones. When those follicles rupture, skin cells and bacteria that are ordinarily present on the skin become trapped in places where they should not be. As a result, the immune system activates, resulting in an even higher inflammatory reaction and pus-filled HS boils.
There are certain known risk factors that can raise the likelihood of HS:
It commonly forms where skin rubs against skin, such as beneath the arms, the vulva, or in the skin folds of obese persons.
High insulin and/or androgen levels, which begin to rise throughout puberty and stimulate pubic and underarm hair growth, among other functions, may also contribute to the problem. In truth, many cases emerge after puberty has ended.
According to the Genetics and Rare Diseases Information Centre of the National Institutes of Health, up to 30% to 40% of patients have a family history of the disease.
Numerous studies have found that smokers are more likely to develop HS, and one recent study published in Dermatology Reports indicated that 67% of participants were current smokers who had smoked for an average of eight years before starting. The less you smoke, like with most things related to smoking, the better off you’ll be.
Is HS unusual?
No, HS is not unusual, despite being mislabeled for decades. The condition’s impression as infrequent “was probably due, in part, to misdiagnosis or under-diagnosis,” according to Dr. Adil, “but also to the shame and stigma that a disease like HS can bring.” People did not seek medical attention immediately.” The fact that the onset of HS typically occurs during puberty, when young people are likely to be self-conscious about their bodies, may possibly contribute to under-diagnosis.
Current estimates place the number of affected Americans at around 1%. This may seem insignificant: However, as Dr. Adil points out, that’s a massive amount for a condition of this severity—HS may be a disfiguring disease. To put this into perspective, approximately the same percentage of people are diagnosed with HS as with IBD (either Crohn’s disease or ulcerative colitis), and even fewer are diagnosed with more widely known conditions, such as multiple sclerosis (less than.5%).
Is HS classified as an STD?
When you have itching, unpleasant, cyst-like pimples or, in the late stages of the disease, excruciating, draining open sores in sensitive areas like the groyne and anus, the question “Is HS an STD?” is quite understandable. The answer, however, is no. According to Dr. Adil, “in some cases, if these patients visit a physician unfamiliar with HS, they may be told they have a sexually transmitted disease,” such as herpes or HPV. Misdiagnoses can and can delay useful and appropriate treatment, aggravating the embarrassment and shame that HS typically causes in patients.
Bottom line: HS is not infectious or contagious, and it is not sexually transferred.
What Are the HS Stages?
“There are three clinical stages to HS,” adds Dr. Adil. Each stage has its own set of symptoms (although early diagnosis and treatment can help manage those symptoms, especially in the earlier stages):
During Stage I, you may detect little (potentially pea-sized), itchy, and painful pimples in the armpits, groyne, near the breasts, and (more commonly in men) around the anus. These may resemble hard cysts or prominent razor pimples.
In Stage II, inflammation and infection have developed, and multiple skin abscesses may occur. Pus-filled tunnels or tracts form beneath the skin; eventually, the abscesses rupture, exposing wounds.
In Stage III, advanced tunnels appear, frequently connecting many lesions. Dr. Unwala believes the injury is permanent at this time. “The tissue has been blown out, and multiple areas have scarring.” She reports that an entire armpit can get inflamed with large boils that are painfully painful and have a horrible scent from the draining pus and fluid.
Is There a Cure for HS?
When you first detected symptoms of HS, how old were you?
12 years old or younger
13 to 20 years old between the ages of 21 and 30 years old
The good news is that there are, and according to Dr. Adil, the sooner you begin therapy, the better your prognosis. In early and moderate cases of HS, doctors have a variety of options for treating infection, preventing new boils, and managing pain.
Finally, in more advanced stages of the disease, surgery may be required. Outpatient procedures requiring tissue excision, which allows the “tunnels” beneath the skin to drain (a technique known as “unroofing”), to more complicated surgeries involving considerable portions of injured skin removed and restored with reconstructive skin grafts are examples.
The level of risk varies according on the surgical procedure. Which is the higher risk? Because HS is a systemic disease, treating one area of skin will not stop the disease from spreading to another. New tunnels will commonly form outside of the treated area.
A recent study found a 35% recurrence rate among HS patients who had surgery.
There are always risks connected with any medical practise. All skin surgeries, for example, include a risk of bleeding or infection, according to Dr. Adil. “Scarring will also result from these procedures, and the appearance of that scarring will vary greatly,” she explains.
There are numerous therapies and medications available to assist control its symptoms.
Topical therapies include antiseptic washes, antibiotic lotions, and keratolytics, which are a form of exfoliant. “Your doctor may prescribe a biologic, which is an injectable medicine that acts on the immune system to reduce inflammation; for example, Humira is a biologic for HS. Oral medications such as antibiotics, retinoids (to assist prevent keratin overproduction), or hormone therapy such as birth control pills may also be prescribed (since doctors believe androgen hormones have a role).
Ayurvedic Treatment – Medicines for HS that involve biologics, antibiotics, or hormone therapy each have their own set of adverse effects, such as affecting the immune system balance (Biologics), affecting the microbiome balance (Antibiotics), or causing hormonal imbalance (Hormone Therapy).
Ayurvedic treatment for hidradenitis suppurativa The goal of treatment is to restore the body’s natural balance by detoxifying it with powerful herbal remedies.
Elite Ayurveda’s treatment for Hidradenitis Suppurativa includes balancing the Kapha and Pitta doshas as well as restoring metabolism harmony. Body detoxification, internal medications to balance doshas, and exterior applications to repair wounds are all part of the treatment.
The treatment consists of herbal mixtures generated based on individual Prakruti and Vikruti analyses.
The most effective therapy usually requires a multidisciplinary approach that involves medicine, surgery, and lifestyle changes (such as quitting smoking, losing weight, and exercising more).
Ayurveda provides a root cause treatment for HS, and many long-term sufferers are no longer experiencing relapses or recurrences.
Who Is the Most Likely to Develop HS?
Hidradenitis suppurativa affects three times as many women as men, and while specialists aren’t sure why, hormones are likely to play a role. Do they comprehend why this is so? No way, not yet. More research, like so much else in HS, is required to determine why certain racial or ethnic groups are more likely to have HS.
Can Diet Aid in HS? (Or worsen the situation?)
To be honest, either is a possibility. And, surprise, there isn’t much data to help us figure out what changes would make a difference. According to the Dermatology article, most responders in a poll of more than 200 patients had reduced at least one food group, and around 86% had eliminated multiple groups. The most common allergens include gluten, dairy, refined sugar, tomatoes, and alcohol. About 30% of those polled said their symptoms had eased, while a few said they had worsened.
Sugars, milk, cheese, and other dairy products, according to the Mayo Clinic, can raise insulin levels, which can contribute to an overproduction of androgens, a type of hormone that appears to be a factor in HS. Similarly, eliminating gluten-containing meals, especially those that need yeast to rise (bread, pizza dough, etc.), may help lesions heal.
What is the secret to identifying your food triggers? Keep a food diary and keep track of your symptoms. Working with a qualified nutritionist may also be advantageous.
Is an HS Treatment Available?
While doctors and researchers work to find answers, the best option for people living with the condition is wise, cautious management, which can keep symptoms under control for many patients.
Ayurveda provides a root cause treatment for HS, and many long-term sufferers are no longer experiencing relapses or recurrences.
Our Prognosis –
EliteAyurveda Clinics has a panel of doctors in many medical disciplines such as endocrine, autoimmune, gynaecology, and so on under one roof. We are well-known for treating chronic and difficult-to-treat illnesses with a holistic and root-cause approach.
To learn more, please contact us.
Hydradenitis suppurativa is a cause of Kapha and Pitta dosha, according to Ayurveda. When the digestive fire (Agni), or Pitta, is out of equilibrium, the Kapha Dosha becomes vitiated, causing metabolism to slow down. Because of the disturbance of fat molecules, they begin to accumulate in muscles and obstruct physiological passages, resulting in painful, swelling sores in the groyne, buttocks, thighs, and armpits.
The goal of hidradenitis suppurativa Treatment in Ayurveda is to restore the body’s natural balance by detoxifying it using effective herbal remedies.
Elite Ayurveda’s treatment for Hidradenitis Suppurativa includes balancing the Kapha and Pitta doshas as well as restoring metabolism harmony. Body detoxification, internal medications to balance doshas, and exterior applications to repair wounds are all part of the treatment.
The treatment consists of herbal mixtures generated based on individual Prakruti and Vikruti analyses. To learn more, please visit our website.
Connect with us to obtain patient testimonials and to chat directly with our patients about their experience in having their ailment treated by us and Ayurveda in general.
Dr. Adil Moulanchikkal, Lead Ayurveda Specialist at EliteAyurveda Clinics, reviewed the medical records. With over 15 years of experience in Neurological, Skin, and Autoimmune Disease treatment.
Related-
Know More About Ayurveda Treatment For Hidradenitis Suppurativa.
GET IN TOUCH

Recent comments