Estimated reading time: 0 minutes
Lichen Planus (LP), characterized by its distinctive itchy, purple lesions, emerges as a complex autoimmune condition, often shrouded in misconceptions. Despite its relative prevalence, myths surrounding LP contribute to unnecessary alarm and confusion among those diagnosed. This discourse aims to clarify these misconceptions, offering insights into LP’s nature, its broader impacts beyond the skin, and debunking common myths to arm patients with accurate knowledge for informed decision-making regarding their health.
Unveiling the Truth Behind Common Myths of Lichen Planus
# Myth: The Contagious Nature of Lichen Planus
Reality: Contrary to some beliefs, LP cannot be spread through touch, shared items, or intimate contact. Its roots lie in an autoimmune mechanism where the body mistakenly targets its own tissues, causing the symptomatic lesions. Factors like genetic predisposition, viral infections, certain medications, and stress are considered potential triggers for this self-directed immune assault.
# Myth: Lichen Planus’s Limited Dermatological Impact
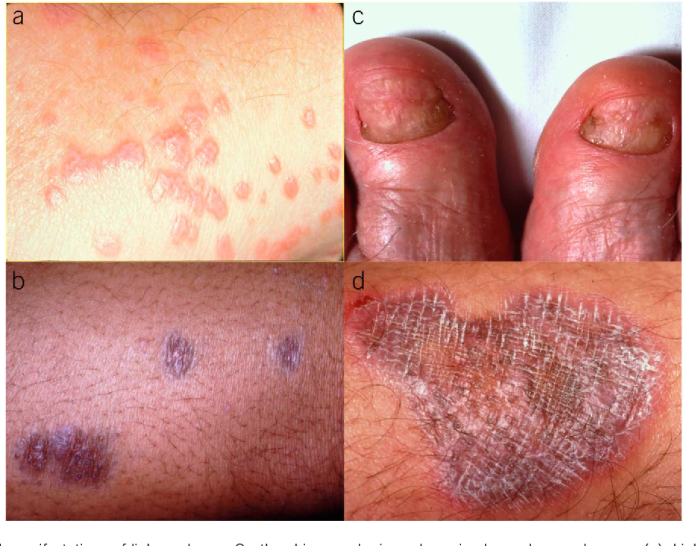
Reality: While the skin is the most visible battlefield, LP’s reach extends to mucous membranes, potentially affecting the mouth, genitals, scalp (leading to hair loss), and nails. Such diversity in manifestation necessitates a holistic diagnostic and treatment approach to address the condition’s full spectrum.
# Myth: The Malignant Potential of Lichen Planus
Reality: LP itself is not cancerous nor a direct precursor to cancer. The condition is marked by an inflammatory immune response rather than malignant transformation. Nevertheless, individuals with Oral Lichen Planus exhibit a slightly elevated risk of oral cancer, underscoring the importance of regular surveillance and preventive care in managing erosive forms of the disease.
# Myth: The Efficacy of Over-the-Counter Remedies for Lichen Planus
Reality: Management of LP often transcends simple over-the-counter solutions, requiring tailored treatments to mitigate its symptoms. This may encompass topical corticosteroids for inflammation, systemic treatments for extensive cases, and specific regimens for oral manifestations. Professional medical guidance is paramount in devising an effective treatment strategy.
# Myth: The Adult-Only Prevalence of Lichen Planus
Reality: Although LP predominantly affects adults, particularly those aged 30 to 60, it does not exclusively afflict this age group. Children can also develop LP, presenting unique challenges in their care and necessitating pediatric-specific management approaches.
# Myth: The Irrelevance of Diet in Lichen Planus Management
Reality: While no diet can cure LP, dietary choices significantly influence inflammation and overall health. Identifying and avoiding foods that trigger or worsen symptoms, especially for those with oral manifestations, alongside incorporating anti-inflammatory foods, can play a supportive role in managing LP.
# Myth: The Inevitable Self-resolution of Lichen Planus
Reality: LP’s course is unpredictable; while spontaneous resolution is possible, many cases persist, experiencing fluctuations in severity. Without intervention, chronic LP can cause considerable discomfort and complications. Proactive management strategies are essential for symptom control and enhancing life quality.
# Myth: The Non-consequential Nature of Stress on Lichen Planus
Reality: Stress acts as a known trigger for LP, among other autoimmune and inflammatory conditions. Integrating stress management techniques into the treatment regimen can mitigate flare-ups, highlighting the interplay between psychological well-being and autoimmune health.
# Myth: The Beneficial Role of Sun Exposure in Treating Lichen Planus
Reality: Sunlight’s effect on LP is not universally therapeutic and may, in fact, provoke lesions in some individuals due to the Koebner phenomenon. Customized guidance on sun exposure and protective measures is advisable for individuals with LP to avoid exacerbating the condition.
Rethinking Lichen Planus: From Myth to Management
The landscape of LP is riddled with myths that obscure its true nature and impact on those affected. By confronting these myths with facts, a clearer picture of LP emerges, emphasizing the need for a nuanced understanding and individualized care. LP’s classification as an autoimmune disorder reveals a complex interplay of genetic and environmental factors, dictating a multifaceted approach to treatment that goes beyond dermatological care to encompass oral health, stress management, and lifestyle adjustments.
Strategic Approaches to Living with Lichen Planus
Patients navigating LP’s challenges are urged to seek reputable medical advice, ensuring a comprehensive evaluation and a tailored treatment plan. The role of diet, while not curative, should not be overlooked, as nutritional strategies can complement medical treatments to control inflammation and support overall well-being. Regular medical follow-ups, especially for those with oral LP, are critical for monitoring disease progression and mitigating cancer risk.
Embracing a Comprehensive Perspective on Lichen Planus
Lichen Planus demands a broad lens, recognizing its potential to affect various body areas and the importance of addressing the autoimmune underpinnings and lifestyle factors contributing to its manifestation. Dispelling myths and fostering an environment of knowledge can empower patients and caregivers alike to tackle LP with effective strategies, aiming not just for symptom relief but for sustained health and quality of life improvements.
In conclusion, demystifying Lichen Planus paves the way for a more informed and proactive patient journey. By debunking prevalent myths and embracing an integrative management approach, individuals affected by LP can navigate their condition with confidence, supported by the pillars of medical science, holistic care, and personalized treatment strategies.
Related-
Know More About Ayurveda Treatment For Lichen Planus.
GET IN TOUCH

Recent comments